Have you ever considered the ups and downs that occur during your day? Speaking literally, you are up and awake during the day and lying down sleeping at night. Speaking figuratively, ups and downs could mean that you experience periods of elevated alertness and arousal compared with your mood when you are tired or relaxed. Asleep, awake, aroused, and relaxed are different brain states, meaning that the brain’s activity is different during each of these periods. Scientists have looked deep inside the brain to understand what sleep is and how rest differs from being alert. This research is especially important for people like doctors, pilots, and shift workers who sometimes must focus and make important decisions with very little sleep. Research on brain states can also help people who have disorders of sleep, attention, and learning.
SLEEP
How many hours of sleep do you get every night? Most people spend one-third of their lives asleep. While that might appear to be a lot of time spent doing nothing, our brains are active while we rest each night. The activity in our brains during sleep is important for brain health and for solidifying memories.
Most people feel tired and unable to focus if they don’t get enough sleep. In some cases, too little sleep can impair a person’s driving as much as drinking alcohol. The long-term effects of lacking sleep also involve many health risks. Several studies in humans have revealed that sleep-deprived people are at increased risk for a wide range of health issues including diabetes, stress, obesity, high blood pressure, anxiety, cognitive impairment, and depression.
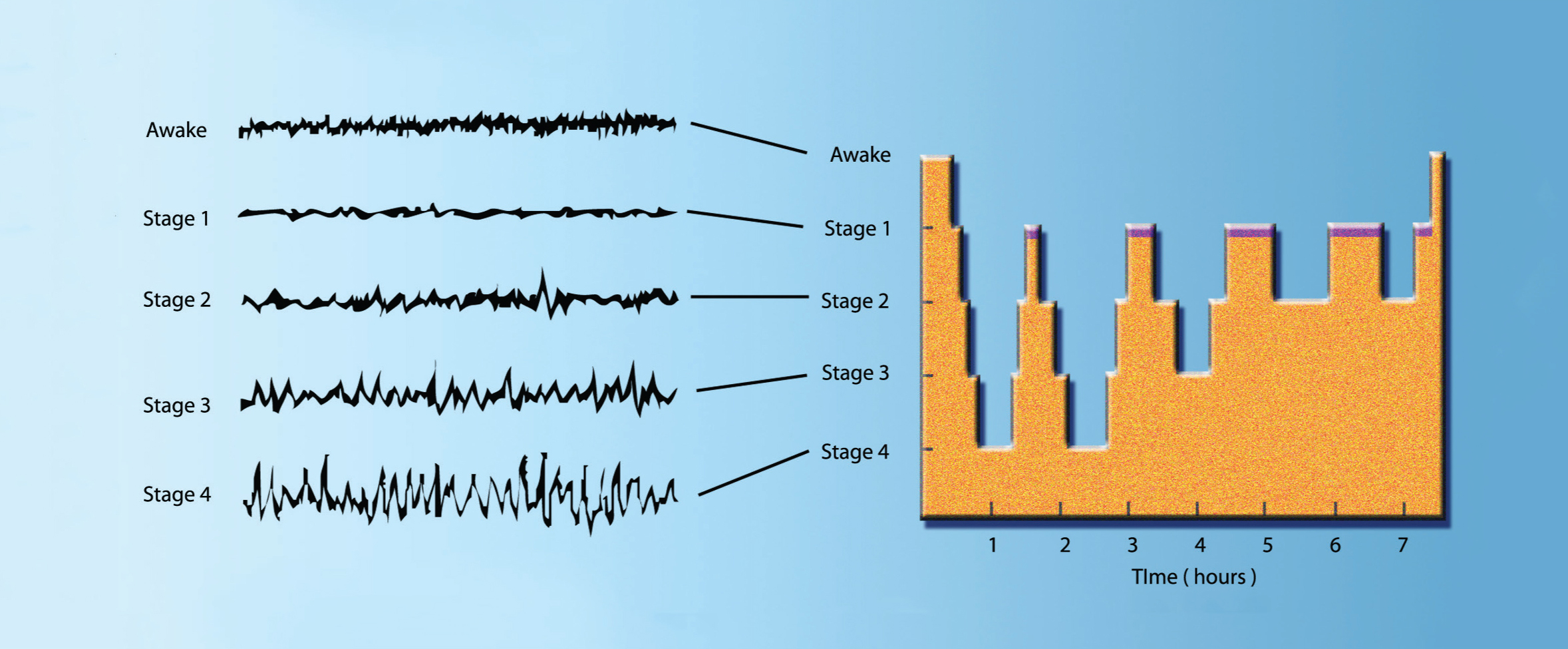
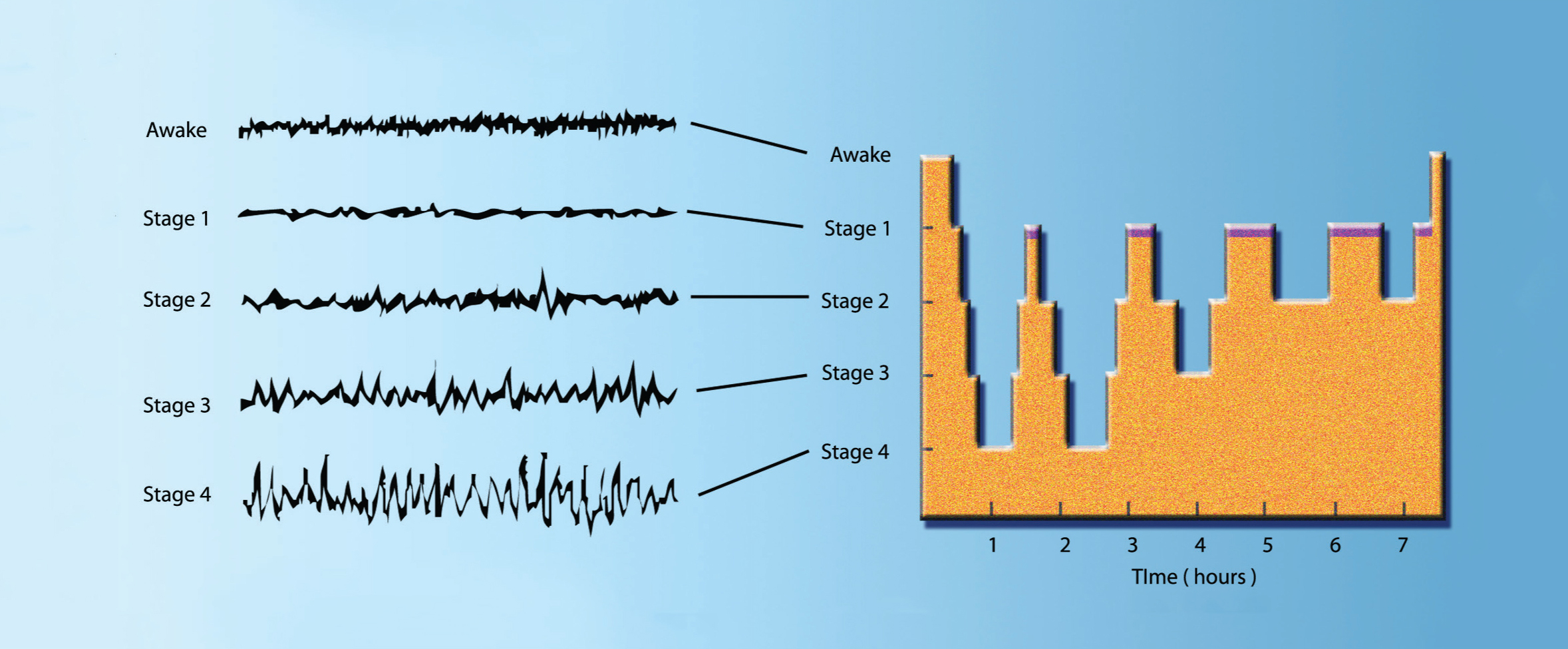
This chart shows the brain waves of an individual being recorded by an EEG machine during a night’s sleep. As the person falls asleep, the brain waves slow down and become larger. Throughout the night, the individual cycles though sleep stages, including REM sleep, where brain activity is similar to wakefulness.
Brain Activity During Sleep
Scientists can measure the brain’s electrical activity using electroencephalography (EEG). Electrodes attached to the scalp detect and record the net electrical activity of hundreds of thousands of cortical nerve cells. When a neuron is active, ions move in and out of the cell, altering the electrical charge across the cell membrane. An EEG detects the net electrical charge produced when neurons increase and decrease their activity as a group, in synchrony. The results are “brain waves” — the cyclic rising and falling of brain activity that can be important indicators of brain function. In sleep studies, scientists now recognize two main states: slow wave sleep (SWS) and rapid eye movement sleep (REM).
SWS gets its name from the high amplitude, low frequency, brain waves in EEG recordings. The high amplitude of slow waves indicates that many cortical neurons are switching their activity in a synchronized way from a depolarized (more excitable) state to a hyperpolarized (less excitable) state and back again. These slow waves appear to be important to sleep function — the longer a person stays awake, the more slow waves they will experience during the SWS state. Slow waves become less frequent the longer the person is asleep. If awakened during SWS, most people recall only fragmented thoughts, not active dreams.
Have you ever seen a cat dreaming — twitching its whiskers or paws while it sleeps? Dreaming happens mainly during REM sleep, which takes its name from the periodic rapid eye movements people make in this state. Brain activity recorded during REM looks very similar to EEGs recorded while awake. EEG waves during REM sleep have much lower amplitudes than the SWS slow waves, because neuron activity is less synchronized — some nerve cells depolarize while others hyperpolarize, and the “sum” of their electrical states is less positive (or negative) than if they acted in synchrony. Paradoxically, the fast, waking-like EEG activity during REM sleep is accompanied by atonia, a loss of muscle tone causing the body to become temporarily paralyzed. The only muscles remaining active are those that enable breathing and control eye movements. Oddly enough, the neurons of our motor cortex fire as rapidly during REM sleep as they do during waking movement — a fact that explains why movements like a kitten’s twitching paws can coincide with dreams.
During the night, periods of SWS and REM sleep alternate in 90-minute cycles with 75–80 minutes of SWS followed by 10–15 minutes of REM sleep. This cycle repeats, typically with deeper and longer periods of REM sleep towards morning. To study sleep disorders, researchers often use mice that have sleep structures qualitatively very similar to humans; however, rodents have shorter and more frequent sleep episodes lasting 3–30 minutes (sometimes longer). Rodents also sleep more during the day and are more active at night. Compare that to human adults, who are typically more active during the day and have one sleep episode at night lasting about 8 hours.
Sleep Regulation
 How does the brain keep us awake? Wakefulness is maintained by the brain’s arousal systems, each regulating different aspects of the awake state. Many arousal systems are in the upper brainstem, where neurons connecting with the forebrain use the neurotransmitters acetylcholine, norepinephrine, serotonin, and glutamate to keep us awake. Orexin-producing neurons, located in the hypothalamus, send projections to the brainstem and spinal cord, the thalamus and basal ganglia, as well as to the forebrain, the amygdala, and dopamine-producing neurons. In studies of rats and monkeys, orexin appears to exert excitatory effects on other arousal systems. Orexins (there are two types, both small neuropeptides) increase metabolic rate, and their production can be activated by insulin-induced low blood sugar. Thus, they are involved in energy metabolism. Given these functions, it comes as no surprise that orexin-producing neurons are important for preventing a sudden transition to sleep; their loss causes narcolepsy, as described below. Orexin neurons also connect to hypothalamic neurons containing the neurotransmitter histamine, which plays a role in staying awake.
How does the brain keep us awake? Wakefulness is maintained by the brain’s arousal systems, each regulating different aspects of the awake state. Many arousal systems are in the upper brainstem, where neurons connecting with the forebrain use the neurotransmitters acetylcholine, norepinephrine, serotonin, and glutamate to keep us awake. Orexin-producing neurons, located in the hypothalamus, send projections to the brainstem and spinal cord, the thalamus and basal ganglia, as well as to the forebrain, the amygdala, and dopamine-producing neurons. In studies of rats and monkeys, orexin appears to exert excitatory effects on other arousal systems. Orexins (there are two types, both small neuropeptides) increase metabolic rate, and their production can be activated by insulin-induced low blood sugar. Thus, they are involved in energy metabolism. Given these functions, it comes as no surprise that orexin-producing neurons are important for preventing a sudden transition to sleep; their loss causes narcolepsy, as described below. Orexin neurons also connect to hypothalamic neurons containing the neurotransmitter histamine, which plays a role in staying awake.
The balance of neurotransmitters in the brain is critically important for maintaining certain brain states.
The balance of neurotransmitters in the brain is critically important for maintaining certain brain states. For example, the balance of acetylcholine and norepinephrine can affect whether we are awake (high acetylcholine and norepinephrine) or in SWS (low acetylcholine and norepinephrine). During REM, norepinephrine remains low while acetylcholine is high, activating the thalamus and neocortex enough for dreaming to occur; in this brain state, forebrain excitation without external sensory stimuli produces dreams. The forebrain becomes excited by signals from the REM sleep generator (special brainstem neurons), leading to rapid eye movements and suppression of muscle tone — hallmark signs of REM.
During SWS, the brain systems that keep us awake are actively suppressed. This active suppression of arousal systems is caused by the ventrolateral preoptic (VLPO) nucleus, a group of nerve cells in the hypothalamus. Cells in the VLPO release the inhibitory neurotransmitters galanin and gamma-aminobutyric acid (GABA), which can suppress the arousal systems. Damage to the VLPO nucleus causes irreversible insomnia.
Sleep-Wake Cycle
Two main factors drive your body to crave sleep: the time of day or night (circadian system) and how long you have been awake (homeostatic system). The homeostatic and circadian systems are separate and act independently.
The circadian timing system is regulated by the suprachiasmatic nucleus, a small group of nerve cells in the hypothalamus that functions as a master clock. These cells express “clock proteins,” which go through a biochemical cycle of about 24 hours, setting the pace for daily cycles of activity, sleep, hormone release, and other bodily functions. The master clock neurons also receive input directly from the retina of the eye. Thus, light can reset the master clock, adjusting it to the outside world’s day/night cycle — this explains how your sleep cycles can shift when you change time zones during travel. In addition, the suprachiasmatic nucleus sends signals through different brain regions, eventually contacting the VLPO and the orexin neurons in the lateral hypothalamus, which directly regulate arousal.
What happens in the brain when we don’t get enough sleep? The second system that regulates sleepiness is the homeostatic system, which makes you feel sleepy if you stay awake longer than usual. One important sleep factor is a chemical in the brain called adenosine. When you stay awake for a long time, adenosine levels in the brain increase. The increased adenosine binds to specific receptors on nerve cells in arousal centers to slow cellular activity and reduce arousal. Adenosine can increase the number of slow waves during SWS. As you get more sleep, adenosine levels fall and slow waves decrease in number. Caffeine acts as a stimulant by binding to adenosine receptors throughout the brain and preventing their interaction with adenosine. As a result, in the presence of caffeine, fewer receptors are available for the slowing influence of adenosine.
People often say they need to “catch up on sleep.” But can you really make up for lost sleep? Normally, the homeostatic and circadian systems act in a complementary fashion to produce a normal 24-hour cycle of sleep and wakefulness. Nonetheless, activating the brain’s arousal system can keep us awake even after a long period of wakefulness — for example, a late-night study session to prepare for an important exam. In normal circumstances, the homeostatic system will respond to the loss of sleep by increasing the duration of ensuing sleep and increasing the number of slow waves during the SWS episodes. As noted above, this rebound slow wave activity correlates with the previous time spent awake and is mediated by adenosine.
Sleep Disorders
The most common sleep disorder, and the one most people are familiar with, is insomnia. Some people with insomnia have difficulty falling asleep initially; others fall asleep, then awaken part way through the night and can’t fall back asleep. Several common disorders, listed below, disrupt sleep and prevent people from getting an adequate amount of sleep.

Simon Fraser University.
Electroencephalography measures brain activity through sensors placed on the head. It can record how the brain reacts to all kinds of stimuli and activities, including sleep.
Daytime sleepiness (not narcolepsy), characterized by excessive feelings of tiredness during the day, has many causes including sleep apnea (see below). Increased daytime sleepiness can increase the risk of daytime accidents, especially car accidents.
Sleep apnea occurs when the airway muscles of the throat relax during sleep, to the point of collapse, closing the airway. People with sleep apnea have difficulty breathing and wake up without entering the deeper stages of SWS. This condition can cause high blood pressure and may increase the risk of heart attack. Treatments for sleep apnea focus on reducing airway collapse during sleep; simple changes that may help include losing weight, avoiding alcohol or sedating drugs prior to sleep, and avoiding sleeping on one’s back. However, most people with sleep apnea require breathing machines to keep their airway open. One such device, called a continuous positive airway pressure or “CPAP” machine, uses a small mask that fits over the nose to provide an airstream under pressure during sleep. In some cases, people need surgery to correct their airway anatomy.
REM sleep behavior disorder occurs when nerve pathways in the brain that prevent muscle movement during REM sleep do not work. Remember that dreaming happens during REM sleep, so imagine people literally acting out their dreams by getting up and moving around. This can be very disruptive to a normal night’s sleep. The cause of REM behavior disorder is unknown, but it is more common in people with degenerative neural disease such as Parkinson’s, stroke, and types of dementia. The disorder can be treated with drugs for Parkinson’s or with a benzodiazepine drug, clonazepam, which enhances the effects of the inhibitory neurotransmitter GABA.
Narcolepsy: An Example of Sleep Disorder Research
 Narcolepsy is a relatively uncommon sleep disorder — only 1 case per 2,000 people in the United States — in which the brain lacks the special neurons that help control the transition into sleep, so that the regular cycling is disrupted. People with narcolepsy have sleep attacks during the day, causing them to suddenly fall asleep, which is especially dangerous if they are driving. The problem is caused by the loss of orexin neurons in the lateral hypothalamus. People with narcolepsy tend to enter REM sleep very quickly and may even enter a dreaming state while still partially awake, a condition known as hypnagogic hallucination. Some people with narcolepsy also have attacks in which they lose muscle tone — similar to what happens in REM sleep, but while they’re awake. These attacks of paralysis, known as cataplexy, can be triggered by emotional experiences and even by hearing a funny joke.
Narcolepsy is a relatively uncommon sleep disorder — only 1 case per 2,000 people in the United States — in which the brain lacks the special neurons that help control the transition into sleep, so that the regular cycling is disrupted. People with narcolepsy have sleep attacks during the day, causing them to suddenly fall asleep, which is especially dangerous if they are driving. The problem is caused by the loss of orexin neurons in the lateral hypothalamus. People with narcolepsy tend to enter REM sleep very quickly and may even enter a dreaming state while still partially awake, a condition known as hypnagogic hallucination. Some people with narcolepsy also have attacks in which they lose muscle tone — similar to what happens in REM sleep, but while they’re awake. These attacks of paralysis, known as cataplexy, can be triggered by emotional experiences and even by hearing a funny joke.
Recent research into the mechanisms of narcolepsy has provided important insights into the processes that control the mysterious transitions between waking, slow wave sleep, and REM sleep states. Orexin (in the lateral hypothalamus) is critical for preventing abnormal transitions into REM sleep during the day. In one study, scientists inactivated the gene for orexin in mice and measured their sleep patterns. They found that mice lacking the orexin gene showed symptoms of narcolepsy. Similarly, humans with narcolepsy have abnormally low levels of orexin levels in their brain and spinal fluid.
Because orexin levels are disrupted in narcolepsy, scientists also began studying neurons that were neighbors to orexin neurons to see what happened if the neighboring neurons were activated in narcoleptic mice. Those neurons contained melanin-concentrating hormone, and stimulating them (using a technique called optogenetics) induced sleep — opposite to the effect of stimulating orexin neurons. A balance between the activation of orexin neurons and their neighboring neurons could control the transition between waking and sleeping. These findings will be important in developing treatments for narcolepsy.
AROUSAL
Think about what happens in your body and mind when you speak in front of a crowd — your brain state is very different from when you are asleep. Perhaps you notice changes in your breathing, heart rate, or stomach. Maybe your thoughts are racing or panicked. Or maybe you are energized and excited to perform for your audience. These are examples of the complex brain state called arousal.
Rather than merely being awake, arousal involves changes in the body and brain that provide motivations to do an action — teaching a class, speaking in public, or focusing your attention. People experience arousal daily when searching for food while hungry, or when talking with other people (social interaction). Arousal is also important for reproduction and for avoiding danger.
The level of arousal varies across a spectrum from low to high. When arousal falls below a certain threshold we can transition from wake to sleep, for example. But under heightened arousal, like intense anxiety, we cannot reach this threshold and we stay awake.
Neurotransmitters
During arousal, the brain must devote resources to specific brain regions, much as an emergency call center redirects resources like ambulances and fire trucks during a fire. Specific types of neurons in the brain regions involved in arousal release multiple neurotransmitters, telling the rest of the brain and the body to be on alert. These neurotransmitters are dopamine (for movement), norepinephrine (for alertness), serotonin (for emotion), and acetylcholine and histamine, which help the brain communicate with the body to increase arousal.
Sensory Input
While neurotransmitters provide the internal signals for arousal, external signals from the outside world — like the bright lights (visual input) and cheering crowds (auditory input) at a stage performance — can also stimulate arousal. Sensory input gets sorted in the brain region called the thalamus. Often called a “sensory clearing house,” the thalamus regulates arousal, receiving and processing sensory inputs from brain regions important in senses like vision and hearing and relaying these inputs to the cortex.
Autonomic Nervous System
Once the brain is aroused, what does the body do? The reticular activating system, in the brainstem, coordinates signals coming from sensory inputs and neurotransmitters to make sense of events in the brain and pass that information to the rest of the body. The reticular activating system specifically controls the autonomic nervous system, which affects heart rate, blood flow, and breathing. By controlling these automatic body processes, the reticular activating system sets up the physical state of arousal, bringing important resources like oxygen and nutrients to parts of the body where they are needed.
Together, the changes that happen in the brain and body during arousal enable us to be alert and focused, which helps us process information quickly. Using this information, we can choose the appropriate emotional response or physical action for a given situation.
Sexual Arousal
Several complex brain systems and endocrine (hormone) systems contribute to sexual arousal and behaviors, but the brain regions, neurotransmitters, and body systems are similar to those involved in general arousal. The distinguishing factor is that sexual arousal also involves hormones such as estrogen and testosterone, which then activate neurons that release the same neurotransmitters that are released during general arousal. Many human and animal studies report interactions between sex hormones and neurotransmitters dopamine, serotonin, GABA, and glutamate. Researchers have also found that brain regions such as the hypothalamus, amygdala, and hippocampus contain many estrogen and progesterone receptors, and brain regions that mediate feelings of reward (nucleus accumbens) and emotions like pleasure (amygdala) motivate sexual behaviors. Overall, the primary involvement of sex hormones is a key in defining the brain state of sexual arousal.
ATTENTION
 If you are paying attention right now, there should be detectable changes in your heart rate, breathing, and blood flow. If that sounds familiar, it’s because those same physiological changes occur during arousal, which is necessary for being alert and paying attention. As mentioned previously, the state of arousal calls for reactions to the environment. To make decisions about what to do, you need to focus on what’s happening in the environment, especially involving anything relevant to your goals. For example, if your goal is to run away from an angry bear, you need to be alert and pay attention to where you’re running so you don’t trip and fall. Scientists have theorized that the state of arousal speeds processing and improves comprehension of environmental details. Otherwise, your brain would need an infinite amount of time and energy to process all of its sensory inputs (sounds, sights, smells, and other feelings), because the environment is always changing.
If you are paying attention right now, there should be detectable changes in your heart rate, breathing, and blood flow. If that sounds familiar, it’s because those same physiological changes occur during arousal, which is necessary for being alert and paying attention. As mentioned previously, the state of arousal calls for reactions to the environment. To make decisions about what to do, you need to focus on what’s happening in the environment, especially involving anything relevant to your goals. For example, if your goal is to run away from an angry bear, you need to be alert and pay attention to where you’re running so you don’t trip and fall. Scientists have theorized that the state of arousal speeds processing and improves comprehension of environmental details. Otherwise, your brain would need an infinite amount of time and energy to process all of its sensory inputs (sounds, sights, smells, and other feelings), because the environment is always changing.
Scientists recognize two types of attention, which involve different brain processes: voluntary attention and involuntary attention.
Focus
Even with multitasking, it is impossible for the brain to process all its sensory inputs. Instead, people focus their attention on one thing at a time. Attention is a fascinating ability, because it enables you to have so much control and the ability to finetune your focus to different locations, times, and topics. Consider the page you are reading right now. Although you can see the whole page, you focus on only one line at a time. Alternatively, you can turn your attention to the past — just minutes ago when you were reading about arousal. Or you can ignore the sentences altogether and focus on the number of times the word “you” occurs on this page. Scientists recognize two types of attention, which involve different brain processes: voluntary (endogenous) attention and involuntary (exogenous) attention.
Voluntary attention happens when you choose what to focus on — like finding a loved one in a crowd. The frontal and parietal cortices of the brain are active when you control your attention or direct it towards a specific object or location. Involuntary attention occurs when something in the environment (like a sudden noise or movement) grabs your attention. Involuntary attention is a distraction from your chosen goals and, in fact, researchers often use distractor objects in attention experiments. Distractors can be emotional, like pictures of family, or non-emotional images that stand out from other stimuli, like a red circle surrounded by gray squares. Brain regions in the right hemisphere, collectively known as the ventral frontoparietal network, form a system that processes new and interesting stimuli that distract you from the task at hand. Research on attention can help us understand visual tasks, learning, child development, and disorders of attention.
Disorders of Attention
 Paying attention for long periods of time, such as a 3-hour lecture, can be difficult for many people. For some people, even focusing for a short time can be hard. Several disorders that affect the ability to pay attention are attention deficit hyperactivity disorder (ADHD), schizophrenia, prosopagnosia, and hemineglect syndrome. It may seem strange to regard schizophrenia as an attention disturbance, but some psychiatric studies suggest that it involves a failure of selective attention. Prosopagnosia, or face blindness, is a cognitive disorder in which a person is unable to recognize faces — even their own family members. The severity of this condition varies, and genetic factors might be involved. Attention disorders have various causes, but we will focus on hemineglect syndrome, caused by damage to the right parietal cortex, a brain region important in involuntary attention.
Paying attention for long periods of time, such as a 3-hour lecture, can be difficult for many people. For some people, even focusing for a short time can be hard. Several disorders that affect the ability to pay attention are attention deficit hyperactivity disorder (ADHD), schizophrenia, prosopagnosia, and hemineglect syndrome. It may seem strange to regard schizophrenia as an attention disturbance, but some psychiatric studies suggest that it involves a failure of selective attention. Prosopagnosia, or face blindness, is a cognitive disorder in which a person is unable to recognize faces — even their own family members. The severity of this condition varies, and genetic factors might be involved. Attention disorders have various causes, but we will focus on hemineglect syndrome, caused by damage to the right parietal cortex, a brain region important in involuntary attention.
Between 50–82 percent of patients who suffer stroke in the right hemisphere experience hemineglect syndrome, also known as spatial neglect and unilateral neglect. In these cases, patients with neglect ignore the left side of their visual field. Sometimes they ignore the left side of the body and the left side of individual objects, as well. Diagnosis of hemineglect syndrome can be done with a pen and paper. For example, patients can be instructed to draw a copy of a picture like a butterfly or a castle, and those patients with hemineglect usually draw only the right half of the picture or leave out details of the left side. Research on patients with hemineglect syndrome contributes to our understanding of rehabilitation after stroke, as well as the role of the right parietal cortex in attention and perception.
REST: DEFAULT MODE NETWORK
 What is the difference between being alert and resting while awake? During times of rest and relaxation, you’re usually avoiding heavy thinking or complicated tasks, and parts of the brain called the default mode network are more active. You may think of the default mode network as a personal lullaby or a playlist that turns on when you are ready to relax. Activity of the default mode network decreases (the lullaby gets quieter) when you start doing or thinking about a demanding task. Human studies using imaging techniques such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) have identified which brain regions belong to the default mode network. These brain areas, which are involved in emotion, personality, introspection, and memory, include frontal brain regions (ventromedial prefrontal cortex, dorsomedial prefrontal cortex, and anterior cingulate cortex), as well as the posterior cingulate cortex, lateral parietal cortex, and precuneus.
What is the difference between being alert and resting while awake? During times of rest and relaxation, you’re usually avoiding heavy thinking or complicated tasks, and parts of the brain called the default mode network are more active. You may think of the default mode network as a personal lullaby or a playlist that turns on when you are ready to relax. Activity of the default mode network decreases (the lullaby gets quieter) when you start doing or thinking about a demanding task. Human studies using imaging techniques such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) have identified which brain regions belong to the default mode network. These brain areas, which are involved in emotion, personality, introspection, and memory, include frontal brain regions (ventromedial prefrontal cortex, dorsomedial prefrontal cortex, and anterior cingulate cortex), as well as the posterior cingulate cortex, lateral parietal cortex, and precuneus.
Although the exact role of the default mode network is unclear, the functions of its “participating” brain regions provide hints about its purpose. Studies on emotion have revealed that activity in the ventromedial PFC is directly related to how anxious a subject feels while performing a task — suggesting that the default mode network may play a role in regulating emotion and mood. Activity in the dorsomedial PFC (a region involved in self-referential or introspective thoughts) increases when a person is at rest and daydreaming. The dorsomedial PFC is also involved in stream-of-consciousness thoughts and thoughts about oneself in the past, present, or future (autobiographical self). The roles of these regions suggest that the default mode network may also function in self-reflection and our sense of self in time.
The posterior brain regions of the default mode network (posterior cingulate cortex, lateral parietal cortex, and precuneus) become more active when remembering concrete memories from past experiences. These brain regions are connected with the hippocampus, which is important for learning and forming memories. Both the hippocampus and the default mode network are more active when a person is at rest in the evening and less active when waking up early in the day. These patterns indicate that the default mode network helps to process and remember the events of the day.
Future studies using electrical recordings from inside the human brain can be paired with fMRI to tell us more about the brain activity patterns of the default mode network and how brain regions coordinate their activity during tasks that utilize the functions of this network. 